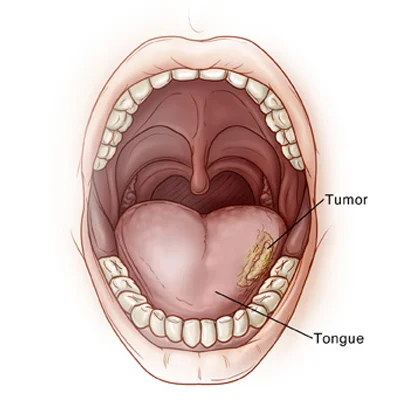
Cancer that occurs on the tongue can be found either on the anterior end(oral end) of the tongue or the posterior end (base of the tongue). The anterior having 4 parts tip, dorsum, lateral borders, and ventral surface out of which the lateral borders get affected by a tumor in most cases. Oral cancer is found out during the initial stages but it is quite advanced when it spreads to the base of the tongue
Stages of Tongue Cancer
The 5 stages of tongue cancer can help the patient plan out his treatment accordingly.
- Stage 0: known as Carcinoma in-situ. This describes the presence of abnormal cells in the surface lining and having a high potential to invade the deeper layers.
- Stage 1: The size of the tumor is less than or equal to 2 centimeters and the cancer cells did not spread to the lymph nodes.
- Stage 2: The size of the tumor is between 2 and 4 centimeters and the cancer cells did not spread to the lymph nodes.
- Stage 3: The tumor is larger than 4cm and without spreading to lymph nodes, or is of any size and had spread to only a single lymph node(less than 3cm).
- Stage 4: It is the most advanced stage. The tumor may be of any size, but it has spread to: Adjacent tissue, skin, or bone. Single lymph node (more than 3cm) or multiple lymph nodes. Distant body parts like lungs etc.
Symptoms of Tongue Cancer :
- Ulceration or lump on the tongue
- Bleeding and numbness
- Reddish or White patches on the tongue
- Lump in the neck
- Pain and difficulty in swallowing
Causes and Risk Factors of Tongue Cancer
Excessive Consumption of Tobacco and Alcohol is the biggest risk factor for tongue cancer. The cancers that are found on the base of the tongue are due to the presence of HPV-16. Chronic irritation by dentures, teeth and poor dental hygiene is another reason for tongue cancer.
Diagnosing Tongue Cancer
- A complete medical history and the patient's history of tobacco and alcohol consumption will help in diagnosis
- Fiber Optic Endoscope is employed to locate any abnormal growth or ulcers on the base of the tongue.
- The biopsy is another way to detect Tongue cancer as it removes a cell or a part of the infected portion to examine it closely. The biopsy varies from condition to condition.
- Neck biopsy will be done if only a bump on the neck is observed
- The complexity and the in depth analysis of the growth will be known through X-rays, CT-Scans and MRI Scans.
Treatment of Tongue Cancer
- The treatment goals of tongue cancer are to eradicate the cancer and restore the form and function of the tongue.
- The treatment modality for achieving these goals in tongue cancer is usually surgery. In case of advanced cancer, surgery should be followed by adjuvant radiotherapy and chemotherapy either alone or in combination.
- The choice of treatment depends on the depth, extent and stage of the tongue cancer.
- Surgery to remove a part of the tongue is known as partial glossectomy whereas advanced cases needed larger tissue removal.
- People with large tissue removal may need a reconstructive surgery to restore the form and function.
Preventing tongue cancer
- Refrain from smoking and consuming any tobacco products.
- Avoid excess drinking of alcohol
- Regular dental check-ups and maintaining good oral hygiene.
- Take a balanced diet rich in fruits, vegetables, Vitamins A, C and E.
Management Of Tongue Cancer
- These are aggressive with early tendency to spread to neck nodes.
- Also they have tendency to relapse after treatment.So early and aggressive treatment ensure cure.
- Following patient presented with non healing ulcer since 2 months.
- Associated with severe pain and earache and neck nodal swellings.
- DIAGNOSIS- Biopsy is done to confirm diagnosis
- IMAGING-CT scan or MRI is done to stage the disease.
Treatment
- Early stage disease is treated with surgery.
- Advanced stagewith multi modality treatment - surgery + radiotheraphy+/-chemotheraphy.
What to expect post surgery
After surgery for tongue cancer, recovery will vary depending on the tumour size, location (tip, lateral border or base of tongue), the extent of tissue removed and whether reconstruction (flap or graft) has been required. Here is a general guide to what patients and families should expect:
- Immediately after surgery you may have a temporary feeding tube or intravenous fluids until the swallowing function recovers and you can safely eat and drink.
- Pain, swelling and discomfort around the surgical area are normal; the team will prescribe appropriate pain relief and may recommend ice / elevation and gentle oral hygiene.
- Eating and speaking may be difficult initially: you’ll begin with a soft or liquid diet and gradually progress to normal food as healing allows and as your speech/swallow therapist guides you.
- If reconstructive surgery was done (e.g., flap repair), you may have specific restrictions on movement, diet and speech; the rehabilitation team will work with you.
- You may require speech and swallowing therapy post-operatively to regain optimal function of the tongue, jaw and neck muscles.
- Regular scheduled follow-up visits will be essential to monitor healing, check for any early signs of recurrence, assess nutritional status, and plan any adjuvant therapy (radiation / chemotherapy) if indicated.
- It may take several weeks to months for full functional recovery, and optimising nutrition, hydration and rest are key to the healing process.
Risks Associated with the Surgery
As with all head and neck tumour surgeries, the procedure to remove tongue cancer carries potential risks. These should be discussed in detail with your surgeon and rehabilitation team. Common risks include:
- Bleeding during or after surgery, requiring close monitoring and possible intervention.
- Infection at the surgical site, or in deeper tissues; prompt management is important.
- Difficulty with swallowing (dysphagia) or aspiration risk, especially if a large portion of tongue or adjacent structures were removed.
- Changes to speech articulation or voice, if tongue mobility or adjacent structures are affected; speech therapy may be needed.
- Altered sensation or numbness in and around the tongue, floor of mouth or neck region, and occasionally altered taste.
- Impact on appearance or function: removal of part of the tongue may require reconstructive techniques, and there may be a period of adjustment to new speech/swallowing patterns.
- The need for adjuvant therapy (radiation and/or chemotherapy) increases the complexity of recovery, and may bring its own side-effects (e.g., mucositis, dry mouth, fibrosis of tissues).
- There is always a small risk of complications with general anaesthesia, as with any major surgery.
Frequently Asked Questions
-
What is tongue cancer and its primary cause?
Tongue cancer is caused by tobacco, alcohol, HPV infection, and genetic factors.
-
What are the common symptoms of tongue cancer?
Symptoms include persistent ulcers, pain, bleeding, difficulty swallowing, and speech changes.
-
How is tongue cancer diagnosed at Amrita ENT Hospital?
We use biopsies, imaging, and advanced diagnostic tools for accurate detection.
-
Does Amrita ENT Hospital provide specialized tongue cancer treatments?
Yes, we offer advanced surgical, radiation, and chemotherapy treatments for effective recovery.
-
What are the treatment options available for tongue cancer?
Surgery, radiation, chemotherapy, and targeted therapy are the main treatment options.
-
How can HPV vaccination help prevent tongue cancer?
HPV vaccines reduce infection risk, lowering tongue cancer chances.
-
What dietary changes help during tongue cancer treatment?
A soft, nutritious, and high-protein diet aids healing and recovery.
-
Why choose Amrita ENT Hospital for tongue cancer treatment?
We offer cutting-edge technology, experienced specialists, and comprehensive cancer care.
-
How does tobacco increase tongue cancer risk?
Tobacco contains carcinogens that damage cells, leading to uncontrolled growth.
-
Are all tongue ulcers a sign of cancer?
No, but persistent ulcers should be checked for proper diagnosis.
